Exam 3 Text: Please let me know of any typos.
ORAL PATHOLOGY
This study set is comprised of the most common lesions in oral pathology.
For each case you will find one or more photographs to illustrate the clinical
features. Radiographs are shown in those cases involving bone. Because this
set is for clinicians, histopathology is kept to a minimum. Each case is
accompanied by a discussion of the cause and treatment.
Our goal is to provide you with a brief and concise study set that will help you learn about the diseases encountered in the practice of dentistry.
They are presented in no particular order.
Table of CONTENTS
1. Developmental non-diseases
a. Fordyce disease
b. foliate papillae/lingual tonsils
c. tori
d. leukoedema
2. aphthous stomatitis
3. herpes virus infection
4. candidosis /candidiasis
5. denture related lesions
a. papillary
hyperplasia
b. denture sore mouth
c.
epulis fissuratum
6. traumatic ulcer
7. irritation fibroma
8. mucocele
9. peripheral fibroma
10. pyogenic granuloma
11. peripheral giant cell granuloma
12. papilloma
13. tobacco related lesions
a. stomatitis nicotina
b. snuff/tobacco keratosis
14. oral melanotic macules
15. amalgam tattoo
16. geographic tongue
17. lichen planus
18. leukoplakia/erythroplakia
19. squamous cell carcinoma
a. dysplasia
b. carcinoma in-situ
20. Periodontal diseases
a. gingivitis
(1) marginal gingivitis
(2) acute necrotizing ulcerative gingivitis
b. periodontitis
(1) adult onset periodontitis
(2) juvenile periodontitis
(3) prepubertal periodontitis
21. dental caries
22. periapical granuloma/periapical cyst
23. condensing osteitis
24. dentigerous cyst
25. nasopalatine duct cyst
26. cementoma
1. DEVELOPMENTAL NON-DISEASES
A. FORDYCE GRANULES (Fordyce spots, Fordyce disease)
This condition appears as flat or slightly elevated, yellow papules on the mucosal surface. Slide #1 is an example. The buccal mucosa shows 1-3 millimeter, slightly elevated yellow plaques. Each plaque is a cluster of sebaceous glands.
Clinical FeaturesCause - Fordyce granules are normal sebaceous glands. Sebaceous glands are normal structures in the skin, but they are regarded as abnormal when found on oral mucosa even though 80% of the population have them.
Histopathology - Slide #2 shows a low-power view. Slide #3 shows a high-power view of the glands. The cells have small nuclei with abundant granular cytoplasm.
Treatment - None required.
B. FOLIATE PAPILLAE/LINGUAL TONSILS
Foliate papillae appear as an area of vertical folds and grooves in the most posterior part of the lateral border of the tongue. They are illustrated in slide #4.
Clinical Features1. Asymptomatic
2. Usually bilaterally symmetrical
3. They are occasionally mistaken for tumors or inflammatory disease.
4. Foliate papillae are vestigial in humans, but they have numerous taste buds and are important in taste perception.
5. Lymphoid tissue is often present in the connective tissue beneath the foliate papillae, and are referred to as lingual tonsils. (illustrated in slide #5)
6. Lingual tonsils Gymphoid tissue) often enlarge during upper respiratory infections causing an enlargement of the foliate papillae.
Cause - These are normal structures.
Treatment - None required.C. TORUS PALATINUS/TORUS MANDIBULARIS
Tori are bony exostoses in the midline of the hard palate and on the lingual aspect of the mandible. Slide #6 shows a palatal torus and slide #7 mandibular tori.
Clinical Features
1. They usually start in young adults and persist throughout life.
2. They seem to have a pre-programmed size and never stop growing when they reach that point. Size ranges from a few millimeters to several centimeters.3. Single lesions may occur in the mandible; however they are multiple and bilateral in 80% of affected individuals. Palatal tori are usually singular and found on the midline of the hard palate. They are often divided by deep grooves. Bony exostoses may occur elsewhere on the alveolar bone, but have no specific name.
4. Palatal tori have been estimated to occur in 20% of the
population whereas mandibular tori affect only 10% of the general population.
5. Some studies show a female to male ratio of 2:1.
Histopathology - Normal bone.
Treatment - Tori seldom produce symptoms; however, when they
interfere with oral prostheses, they should to be removed. Tori
invite trauma and traumatic ulcers of the mucous membrane that
covers tori are slow to heal.
D. LEUKOEDEMA
This condition appears as white to slate gray, opaque discoloration of the oral mucosa. Slide #8 is an example
of leukoedema on the buccal mucosa.
Clinical Features
1. Occurs chiefly on the buccal mucosa.2. The mucosa may have a folded or wrinkled appearance - This may completely or partially disappear when the mucosa is stretched.
3. It is more common in blacks than caucasians, and more common in men than women.
4. It is more prominent in smokers.Cause - Leukoedema is a variation of normal that should not be confused with premalignant leukoplakia. A rare inherited condition,white sponge nevus, may clinically resemble leukoedema.
Histopathology - There is an increase in the thickness of the epithelium, intracellular edema of the spinous layer. a superficial parakeratotic layer, and broad, irregularly elongated rete ridges.Treatment - None required.
2.
APHTHOUS STOMATITIS
(canker sore, recurrent aphthous stomatitis, (RAS) )
Slides #9 and #10 show typical lesions. A single lesion is ordinarily
about 2-5 mm in diameter. Small lesions less than 0.5 cm are called minor
aphthae, whereas larger lesions (more than 0.5 cm) are referred to as major
aphthae (slides # 11 and # 12). The central, yellowish-white area represents the
zone of ulceration and necrosis. The surrounding red halo is the area of
acutely inflamed, non-ulcerated mucosa.
1. RAS occurs in all ages. it is more common in children and young adults and generally decreases in frequency with advancing age.
2. Usually occurs as a single lesion, but patients may have multiple lesions. Slides # 13 and # 14 show patients with multiple lesions on the soft palate and lateral border of the tongue.
3. Abrupt onset, painful and last about 7-10 days.
4. Occurs most commonly on the "movable" mucosa. (i.e.
5. The typical patient with RAS usually has recurrent episodes. The duration between recurrences is extremely variable ranging from a few days to several months.
6. The incidence in the general population has been estimated at 20% while in select groups such as students it has been as high as 50%.
Cause - The cause remains unknown, although a multifactorial cause is probable. The current thinking is that aphthous stornatitis is a disease of immune origin, most likely a type IV cell mediated immune injury. Both bacterial and viral infections have been implicated in the past, but have recently been regarded as unlikely causes. Nutritional deficiencies of vitamin B 12, folate and iron are implicated but replacement therapy is not uniformly successful. Aphthous ulcers are also more common in women during the menstrual cycle and after trauma to the mucosa. Lastly RAS has also been associated with specific MHC antigens, suggesting an inheritable component.Histopathology - Non-specific inflammation and ulceration. In the early stages there is a predominance of lymphocytes.
Treatment - Topical applications of steroids such as triamcinolone acetonide(Kenalog) or fluocinonide(Lidex) is probably the best treatment for patients with few lesions. In severe disease, oral prednisone is recommended.Comment - The diagnosis is usually made by a history of recurrent ulcers and their clinical appearance. If ulcers last for more than two weeks and there is no history of recurrent lesions, a biopsy may be necessary to rule out other diseases. Patients with a history of RAS are susceptible to developing aphthous lesions at sites of trauma. This is known as the Koebner reaction or isomorphic response
Good review articles of aphthous are:
1. Clinical and Experimental Dermatology, # 16:pg. 235-243, 1991.
2. Current Problems in Dermatology, Julv-Aug. 1991
3. ORAL HERPES VIRUS INFECTION
Two types:
(A) Widespread infection of oral mucosa called "primary herpetic gingivostomatits", or first episode herpetic stomatitis.
(B) Localized infection usually found on the vermilion of the lip and adjacent skin. This type is called "herpes labialis", or secondary " herpes. Less cornmonly, secondary herpes occurs on the hard palate.
A. Primary herpetic gingivostomatitsSlides # 15, # 16 and # 17 show a patient with the "first episode" type of herpes virus infection. Each lesion starts asa small vesicle (blister) that soon bursts and becomes a shallow ulcer. Adjacent lesions mayjoin to produce larger, irregularly shaped areas of ulceration. Extensive inflammation in the surrounding mucosa produces redness and swelling.
Clinical Features1. Most commonly found in children 3-10 years old, but may occur at any age.
2. Acute onset with multiple lesions. Gingivitis usually appears before vesicles develop on other mucosal surfaces.
3. Pain and fever up to 103 degrees F with lethargy.4. Inability to eat and drink may lead to dehydration, especially in children.
5. A "self-limiting" disease lasting about 10 days. In immuno-compromised patients herpes simplex infection way be life threating and requires treatment.
Cause - a 130-180 millimicron DNA virus called herpes simplex virus (also: herpes virus hominis). Other important human pathogens of the herpes family include varicella-zoster virus that causes chickenpox in children and herpes zoster (shingles) in adults. Examples of zoster are shown in slides # 18 and # 19. Also, cytomegalic virus (CMV) belongs to the herpes family as does the Epstein-Barr virus. The CMV is a major pathogen in HIV and other immunocompromised patients. The EB virus is thought to cause infectious mononucleosis, Burkitt's lymphoma, nasopharyngesl carcinoma, and hairy leukoplakia in HIV patients.
Histopathology - The herpes virus is cytolytic; as the virus
replicates, the infected cell dies. The nuclei of infected cells swell and
clusters of intranuclear virus particles may be large
enough to be seen with an ordinary microscope. These clusters or
inclusion bodies are also called Lipschutz bodies. As infected
epithelial cells die, cell attachments are lost and there is an influx
of serum and leukocytes. The result is the formation of an
intraepithelial vesicle. Virus infected cells float in the
vesicle fluid and may fuse to form characteristic multinucleated
giant cells.
Slide #20 is normal oral mucosa for comparative purposes.
Slide #21 is a drawing depicting the normal tissue shown in slide
#20. Slide #22 is a herpes vesicle. A thin roof remains on the
vesicle and the basement membrane is obscured by necrosis of
epithelial cells. There is a heavy leukocytic infiltrate in the lamina
propria. Slide #23 is a drawing of the vesicle to help interpretation.
Diagnosis- As stated above, the herpes virus produces a
characteristic cytopathogenic effect in infected epithelial cells.
They become large and multinucleated as seen in slide #24. Slide
#25 is a drawing of the cells seen in slide #24. A cytologic smear is
a quick, painless and inexpensive way to diagnose herpes. The
cytologic smear is obtained by breaking a vesicle and collecting the
fluid on a glass slide. It is stained in the usual manner (Pap stain).
A viral culture is a more accurate method of diagnosis but is more
expensive, takes 3-7 days and is not readily available in the
general practice setting.
Treatment - Treatment is palliative. Mouthwash consisting of
equal portions of Kaopectate and elixir of Benadryl provide some
relief from pain as does Zylocaine viscous. The efficacy of Zovirax
(acyclovir) is questionable. Although the benefits of this drug in
herpetic encephalitis and in immunocompromised hosts is
undeniable, as of this writing there are no published reports
indicating its usefulness in primary gingivostomatitis in hosts with
normal immune systems. (See comments on treatment under
herpes labialis).
Comment - Biopsy is seldom necessary because diagnosis can be
arrived at clinically or confirmed by cytology or culture.
B. Secondary herpetic infections (herpes labialis) (recurrent herpes)
Slides #26 and #27 show typical examples of herpes labialis.
Slides #28 and #29 show secondary herpes of the hard palate.
Clinical features
1. More common in teenagers and adults.2. Occurs most commonly on vermilion border of the lip and adjacent skin, less commonly on hard palate.
3. Sudden onset, little pain, no constitutional symptoms such as fever. A prodrome of itching or burning is sometimes present.
4. Lesion occurs as a small patch of vesicles that break, quickly scab over, and heal in about 10 days.
5. Disease occurs in cycles and is thought to be triggered by trauma, exposure to sunlight, citric fruits, menstruation and febrile illnesses. (thus the name "fever blisters"). There is no scientific evidence that dietary factors and menstruation are actually triggering agents.
Cause - Herpes simplex virus, type I. In some studies, 20-40% of labial lesions have been found to be caused by type II virus, most likely transmitted by oral-genital contact.Histopathology - Same as primary herpetic gingivostomatitis.
Treatment - Except for immunocompromised patients there is no highly effective treatment for either primary or second episode herpes simplex. Most treatment is centered on making the patient comfortable since the disease is self limiting. Topical anesthetics are usually sufficient in controlling the pain.
Acyclovir (Zovirax) in either topical or tablet form is not
generally recommended for either primary or second episode
oral infections. Studies have shown only a very slight clinical
benefit. Acyclovir tablets 200mg five Limes daily maybe effective in preventing recurrent episodes when
they are taken
prior to precipitating factors. A good reference is New England Journal of Medicine #327: pg 82-89. 1992
Comment - There are essentially two main types of oral herpes
simplex infection. The "primary" form develops in those who have
not had previous exposure to the virus and have little or no immunity to it. The "secondary" form is thought to occur in people
who have some immunity because of previous exposure. The primary infection is a one time episode whereas patients may
have multiple secondary episodes. Both forms are highly
contagious. Slide #30 shows the finger of a dentist with herpes he
contracted from a patient with oral herpes. This has become rare
in dentists since the advent of universal precautions.
Herpes virus is both
epidermotropic and neurtropic (skin loving
and nerve loving). When the virus enters skin or mucosa, through a small break in the surface, it travels through nerve
trunks to the nearest regional ganglia such as the trigeminal
ganglia. There it may exist in a dormant (latent) stage forever. Periodically, the virus may migrate from the ganglia to skin or
mucosa where it produces recurrent lesions.
Good review articles on Herpes include:
"New England Journal of Medicine, "
Vol. 314 # 11, pg. 686-69 1. March 13, 1986
Vol.314 # 12, pg.749-757, March.20, 1986
Vol. 327# 11, pg. 782-789, Sept. 10, 1992
|
A
COMPARISON OF APHTHOUS
STOMATITIS
AND HERPETIC
STOMATITIS
APHTHOUS HERPES CAUSE
Unknown
DNA virus called herpes virus hominis or herpes simplex (herpes type I) TYPE
OF
Single or multiple Primary form causes acute febrile LESION
ulcers exclusively illness characterized by diffuse stomalitis
on oral mucosa
mostly
on chiefly in children but sometimes
"loose" mucosa
such as
in adults. Secondary form characterized.
labial and buccal
mucosa. by recurrent lesions on vermilion
Typically is a disease of lip and adjacent skin. Primary form
characterized by is a "one-shot" disease. (ie,
you don't multiple recurrences. get it again except in very rare cases). SIGNS
No fever, malaise, or Fever, malaise. and leukocytosis
are
leukocytosis. present in primary type and absent in
secondary type. HISTOLOGY
Ulceration of oral Intraepithelial
vesicle with intranuclear
mucosa
with nonspecific viral inclusion bodies
(Lipschutz
inflammation. bodies). Vesicles break and an ulcer
forms. Lesion may then resemble an
aphthous
lesion. TREATMENT
For patients with just Primary
herpes -
topical anesthetics to
a few lesions, we prefer
alleviate pain. Acyclovir
is useful in
topical application of Immunocomprised,
but of limited
steroid or over the value in those with a normal immune
counter preparations system.
containing topical
anesthetics or anti- Secondary
herpes- Topical anesthetic
inflamatory
medications. and /
or over the counter preparations
For severe or widespread maybe helpful in alleviating pain.
ulcerations we use systemic Acyclovir
is of limited value. (see
steroids such as a 4 mg references)
Medrol
dosepak,
with or Most over the counter preparations
without an anesthetic contain benzocaine.
mouthrinse.
Patients must be cautioned
about the possible adverse
effects of systemic steroids. |
4. CANDIDOSIS/CANDIDIASIS
(thrush, moniliasis)
This is an infection caused by the fungus Candida albicans. This
organism can be found in up to 50% of healthy people as normal flora. It
is frequently the cause of infection in areas other than the mouth such
as skin, G-1 tract and vaginal mucosa. This discussion is limited to
oral lesions.
Clinical Features
1 . Candidiasis occurs at any site in the mouth. Because of
inflammation, the mucosa becomes red. The fungus colonizes superficial epithelium and in severe cases causes
surface necrosis.
The mixture of fungi and dead tissue appears as a white membrane that can be wiped off easily, leaving a raw and
easily bleeding surface. These lesions are mildly painful.
3. This disease is prevalent in infants, immunocomprised and
debilitated patients patients taking antibiotics (antibiotics eliminate bacteria that compete with Candida). The patient in slide #31 had leukemia and was taking drugs that suppressed his immune system. The patient with palatal candidiasis in slide #32 was taking prednisone for the treatment of asthma. 4. Oral candidiasis is a frequent occurrence in AIDS patients and may
be seen in asymptomatic HIV antibody positive patients. An asymptomatic HIV positive male homosexual with candidiasis of
the ventral tongue is seen in slide #33 and slide #34 shows white lesions of the lateral tongue that cultured positive for candidiasis
in an AIDS patient.
Cause - Candida albicans, rarely other species such as C. tropicalis.
Comment - While removable white plaques are the most common clinical
presentation of candidiasis several other forms of the disease may exist
in the oral cavity.
*Angular Cheilitis- these are maceratious or fissures that occur at
labial commissures. Topical antifungal preparations of nystatin or
ketoconazole are highly effective treatments. (Slide #37)
*Chronic Atrophic Candidiasis- this is a diffuse usually painful
redness that most commonly occur beneath removable dental appliances.
White plaques are rarely present. This condition under dentures is also
known as denture sore mouth (see slide #42). Chronic atrophic
candidiasis is seen in HIV patients, and is not related to removable dental
appliances.
5.
DENTURE RELATED LESIONS
A. PAPILLARY HYPERPLASIA OF THE PALATE
Slides #38 and #39 show typical patients with this
lesion. The palatal mucosa has a red, papillary texture.
Clinical Features
1. Occurs primarily in people who wear dentures or other
removable appliances.
2. Usually asymptomatic and of long duration (months to years).
Cause- Most commonly associated with wearing dentures 24 hours per day. Patients should be advised to leave dentures out at night.
Histopathology - The mucosal surface is thrown into multiple papillary folds as seen in slide #40. Submucosal connective tissue
shows mild edema, infiltration of inflammatory cells, chiefly lymphocytes and plasma cells, with
fibrous hyperplasia. Slide #41 is a high-power view that shows the edema and chronic
inflammatory cell infiltrate in the lamia propria. These changes support an inflammatory cause.
Treatment - Eliminate the source of inflammation which is often a poorly fitting denture that is not removed at
night. Lesions that do not respond or that interfere with the fit of denture may require surgical removal.
Secondary candidiasis is often present.
B. DENTURE SORE MOUTH
(chronic atrophic candidiasis, atropic denture Stomatits.)
Slide #42 shows a typical patient with this lesion. The mildest form of denture sore mouth (DSM) appears as small, localized and asymptomatic red spots on the posterior palatal mucosa. As the condition worsens, large areas may coalesce and become bright red. This is classic DSM. Because of similar appearances and location, some feel that DSM is a prelude to papillary hyperplasia.
Cause - Most evidence supports Candida albicans as the cause... and therefore it is often referred to as chronic atrophic candidiasis. Factors other than Candida albicans are probably involved, but it is difficult to assess the role of denture trauma and bacteria. In the past it had been theorized that allergy to denture base material was the cause of denture sore mouth, but there is little evidence to support this view.
Treatment - Antifungal drugs bring about remission in most cases, but recurrences are common when treatment is discontinued. Since organisms have been shown to colonize the tissue Surface of the denture, sterilization of the denture with fungicide is also indicated.
C. EPULIS FISSURATUM
Slides #43 and #44 are clinical photographs of epulis
fissuratum. The lesion usually occurs in or near the vestibule in the anterior maxillary or mandibular mucosa. The usual size
is about 1-2 cm, but they may be larger. They may be of normal color or slightly red, ulcerated, and are usuallv
bilobed.
Clinical Features
1. Asymptomatic and of months duration. May be painful if ulcerated.2. Occurs exclusively in those with removable prostheses.
3. Usually bilobed, or multilobed with the denture flange
fitting in the crevice that separates the lobes. Slide #44
shows a leaf-like epulis
fissuratum with several folds.
Cause - Chronic irritation from over-extended denture flange.
Histopathology - Fibrous connective tissue hyperplasia with or without epithelial hyperplasia. Usually shows acute and/or chronic inflammation and ulceration is common.
Treatment - Reduction of the denture border, and surgical removal when necessary.
6. TRAUMATIC ULCER
An ulcer by definition is a localized area on skin or mucosa in which the surface epithelium has been destroyed. The shape and size of traumatic ulcers are so variable as to defy a simple description. They are usually painful and of short duration, and often the result of physical, chemical or thermal trauma. Slide #45 shows a traumatic ulcer in a patient who bit his tongue. Slide #46 is a traumatic ulcer on the alveolar ridge of an edentulous patient. This ulcer was the result of a burn caused by hot compound impression material.
Clinical Features
1. There is a tremendous range in size, from a millimeter to several centimeters.2. They occur on any surface and are usually painful.
3. The ulcer is covered by a mixture of fibrin and inflammatory exudate including dead and dying leukocytes.This fibrous exudate appears yellowish-white clinically. Inflammation in the surrounding mucosa. usually produces a halo of erythema.
Cause - Any kind of mechanical, thermal or chemical trauma severe enough to cause necrosis of surface epithelium. Common causes of traumatic ulcers include biting injuries, thermal burns, and strong chemicals. Dentures are also a frequent cause of traumatic ulcers.
Histopathology -The histopathic features are simple. The surface epithelium is missing and replaced by a fibrinous exudate. Inflamed granulation tissue forms the ulcer bed beneath the exudate.
Treatment - Remove the cause of the trauma. Healing will occur
within 1-2 weeks. If it does not heal, you must suspect your
diagnosis was wrong. Biopsy is then indicated. Remember, early
squamous carcinoma may clinically resemble a non-specific ulcer.
(traumatic fibroma)
7. IRRITATION FIBROMA
Traumatic fibroma is a dome-shaped, soft tissue mass most
commonly found on the buccal mucosa. The color is usually the same as
Clinical Features
1. They are among the most common oral soft tissue lesions.
2. Found in all age groups, but most common in adults.
3. Asymptomatic. Patients are generally aware of the lesion being present months to years with little change.
4. Size is a few millimeters to 2.0 cm, seldom longer.
5. Usually found on buccal mucosa. along the line of occlusion, on lower lip mucosa and sometimes the tongue.
Cause - The presumed cause is trauma. Accidental biting probably accounts for most of these lesions.
Histopathology - There is hyperplasia of fibrous connective tissue with abundant collagen formation. Mucosal epithelium covering the fibrous nodule ranges from normal to atrophic, Slide #49 is a "life size" traumatic fibroma. The thin, blue rim is the surface epithelium and the balance of the lesion is collagenous fibrous connective tissue.
Treatment - Surgical removal is the treatment of choice. They are self-limiting but they do not regress once trauma is removed. Other tumors may clinically resemble irritation fibromas but will exhibit progressive growth.
8. MUCOCELE
(mucous escape phenomenon)
A mucocele is a collection of saliva (mucus) within the substance of the oral mucosa. Slide #50 is an example of a mucocele on the lip.
Clinical Features
1. They occur in all ages, with no sex preference.2.They are found most commonly on the lower lip, buccal mucosa, and occasionally the ventral surface of the tongue, rarely in other salivary gland bearing areas such as the floor of the mouth, and retromolar pad.
3. They are soft elevations whose color ranges from that of normal mucosa to light blue.
4. Frequently, lesions flucuate in size. Some lesions may completely disappear, then reoccur.
Cause - Severance of the duct of a minor salivary gland allows the escape of saliva into surrounding connective tissue. A mucocele in the floor of the mouth is called ranula. An example of a ranula is seen in slide #51.
Histopathology - There is accumulation of saliva in mucosal connective tissue. The connective tissue usually tries to "wall-off' the saliva by forming a layer of fibrous connective tissue at the periphery. Within the mucus lake and the surrounding connective tissue, there is infiltration of leukocytes, mainly neutrophils and histiocytes (macrophages). Mucoceles are NOT lined by epithelium. Slide #52 is a drawing of mucocele. A mucous retention cyst is a similar lesion that is lined with ductal epithelium.Treatment - Surgical excision of the mucocele deep enough to include the underlying salivary gland that is feeding it.
9. PERIPHERAL FIBROMA
(peripheral ossifying fibroma)
Slide #53,
#54 and #55 are examples of this lesion.
Clinical Features
1. More common in females and favors teenagers and young adults.
2. They occur exclusively on the gingival mucosa almost always adjacent to teeth. They are most common in the anterior maxillary region.
3. They are asymptomatic, grow slowly, and have been present for a few months before the patient seeks help.
4. Most lesions are less than 1.5 cm but lesions up to 6 cm have been reported. A large peripheral fibroma is seen in slide #54.
5. Color is normal to red: they usually are firm, but not bony hard. Many become ulcerated.
6. The lesion may produce, pressure resorption of underlying bone and the adjacent teeth may be pushed apart. An example is shown in slide #55.
Cause - Unknown. A reactive lesion, not a neoplasm.Histopathology - The bulk of a peripheral fibroma is moderately cellular connective tissue that frequently containing foci of bone, cementum, or dystrophic calcification. When inflammation is present, plasma cells predominate. Slide #56 is a low-power view showing some calcifications in the superficial connective tissue. Slide #57 shows bone formation and in slide #58, one can see several droplets of cementum.
Treatment - Excision down to periosteum. The lesion is benign,
but will recur if incompletely excised. Recurrence rates
of
14-16% are reported.
(granuloma pyogenicum, pregnancy tumor)
The pyogenic granuloma is a red, nodular overgrowth of granulation tissue that arises from a mucosal or skin surface. You will recall that granulation tissue is reparative tissue consisting chiefly of endothelial cells that form new capillaries and fibroblasts that synthesize collagen and ground substance.
Clinical Features1. Occurs in all ages and both sexes. There is a higher incidence during pregnancy, thus the name "pregnancy tumor". Slides #59 and #60 are of pyogenic granulomas in pregnant women. They occur in men as seen in slide #61.
2. Pyogenic granulomas occur on any mucosal or skin surface, but the mouth is the most common place for them. They are most often occur on the gingiva.
3. Size ranges from a few millimeters to about 1.5 cm. They seldom exceed this size. Separation of teeth is uncommon in pyogenic granuloma.
4. They are usually redder than surrounding tissue due to increased vascularity, and they bleed easily.
5. Duration ranges from a few weeks to a few months.
Cause - The stimulus that provokes this overgrowth of granulation tissue is unknown although mild trauma and infection are suspected.Histopathology - An exuberant mass of granulation tissue. There are many new capillaries and venules growing in an edematous and inflamed fibrous connective tissue. In spite of the name pyogenic granuloma, these lesion usually are not "pyogenic" (pus producing). Slide #62 shows a low-power view. Capillaries are seen among the edematous connective tissue. Inflammatory cells can also be seen.
Treatment - Conservative excision, recurrence rate is low.
11. PERIPHERAL GIANT CELL GRANULOMA
(peripheral giant cell tumor, peripheral giant cell reparative granuloma)
The peripheral giant cell granuloma appears as a nodular, red or purple, soft tissue mass arising exclusively on the gingiva or alveolar mucosa. Clinically, they may resemble pyogenic granuloma and peripheral fibroma. Slide #63 shows a typical peripheral giant cell tumor. Slide #64 shows a larger one. Peripheral giant cell granulomas may sometimes be seen in edentulous areas. Slide #65 is an example. The word "peripheral" is attached to the name of this lesion to indicate its origin in soft tissue outside of bone. (A histologically similar lesion occurs inside bone and is called "central giant cell granuloma").
Clinical Features1. Occurs exclusively on gingiva. Most lesions occur between ages 10-60 with an average age in the United States of about 30.
2. Usual size is less than 1.5 cm but they are often much larger.
3. Usually redder than surrounding mucosa.
4. Asymptomatic, duration is usually several weeks to a few month.
Cause - Unknown.
Histopathology - Slide #66 is a low-power view. The surface epithelium is intact and the tumor can be seen in the underlying connective tissue. Slide #67 is a high-power view, a multinucleated giant cell is seen. A few erythrocytes (red dots) can also be seen. The rest of the cells are fibroblasts, the chief cell of this lesion. Usually one can find a few inflammatory cells. Hemosiderin pigment (from hemoglobin breakdown) may also be found. It seems likely that giant cells arise from fusion of macrophages. Immunohistochemical studies show that the antigenic markers for macrophages and the giant cells in the lesion are similar.Treatment - Excision down to periosteum. Recurrence rate is about 10%.
Comparison of Peripheral Fibroma, Pyogenic Granuloma, and Peripheral
Giant Cell Granuloma
The age, sex, and race of the patient does not help to distinguish between these lesions clinically. Usually, pyogenic granuloma and giant cell tumor are fairly red especially the pyogenic granuloma. This is because of rich vascularity. Peripheral fibroma may be red, but often are of the same color as surrounding mucosa. Because the fibroma is composed of compact fibrous connective tissue, and often contains bone, it is more firm to palpation.The only sure way to tell these three lesions apart is microscopic examination. Pyogenic granuloma consists of inflamed granulation tissue, whereas giant cell granuloma consists of cellular fibrous connective tissue and histiocytic proliferation with considerable vascularity and most obvious of all, multinucleated giant cells. The peripheral fibroma is a fibroblastic proliferation with or without bone and/or cementum production.
Don't forget! Peripheral giant cell granuloma and peripheral fibroma are found exclusively on gingival or alveolar mucosa. Pyogenic granuloma occurs commonly on gingiva, but may be found on any skin or mucosal surface.
12. PAPILLOMA
(squamous papilloma)
Slide #68 shows a typical papilloma on the lip and slide #69 is a
papilloma on the lingual frenulum. Papillomas are benign proliferations of
squamous epithelium. They are said to be the most common epithelial
neoplasm in the mouth, but there is some question whether a papilloma should
be considered hyperplastic or neoplastic. There is no evidence that papillomas
are premalignant.
Clinical Features
1. Occurs in all ages and in both sexes.
2. Soft palate is the most common site.
3. They are asymptomatic.
4. Size ranges from a few millimeters to a centimeter. (average less than 1 cm.)
5. They usually occur as solitary lesions, but sometimes a patient will have multiple lesions.
6. They resemble little "cauliflowers" attached to the surface of he mucosa. They may be whitish or normal mucosal color.
Cause - Viral origin has always been suspected, but studies are still inconclusive. Antigens of the human papilloma virus (HPV) have been identified in approximately 50%. There have been over 60 types of (HPV) identified. Oral papillomas are associated with types 2,6, and 11. The same virus may be seen in lesions similar to the papilloma such as verruca vulgaris and condyloma accuminatum. Condylomata are caused by HPV types 6 & 11. (verruca vulgaris is the common skin wart and condyloma is a genital wart)
Histopathology - Multiple fingers of squamous epithelium extend above the mucosal surface. Each "finger" has a core of fibrous connective tissue that is continuous with the connective tissue at the base of the lesion. Slide #70 is a low-power, cross-section of a papilloma. The exophytic and papillary structure is easily seen.
Treatment - Conservative surgical excision, recurrence is rare. Because they are harmless, removal is elective.
13. TOBACCO RELATED LESIONS
A. STOMATITIS NICOTINA (nicotine stomatitis, smokers palate)
This lesion occurs on the mucosa of the hard palate and to a lesser extent the mucosa of the soft palate. It is found exclusively in heavy smokers. Pipe smoking is usually the greatest offender Slide #71 is a typical case.
Clinical Features
1. Mostly in adult males.2. Asymptomatic. Patients are usually unaware of it.
3. The palatal mucosa is white and is criss-crossed by fissures. Small papular elevations with a red center are scattered throughout the lesion. They are the orifices of minor salivary gland ducts.
Cause - This lesion is caused by smoking, chiefly pipe and cigar smoking. Similar lesions may be caused by frequent drinking hot liquids.
Histopathology - Slide #72 is a low-power view of one of the papules. The mucosa is hyperkeratintized and is hyperplastic with mild papillomatosis. Chronic inflammation, especially around the orifices of minor salivary gland ducts cannot be seen at this magnification. We do not usually biopsy this lesion because the diagnosis can be arrived at by visual inspection.
Treatment - This condition usually disappears after the discontinuance of smoking. This lesion is NOT premalignant.
B. SNUFF/TOBACCO KERATOSIS
This lesion develops on the mucosa where smokeless tobacco is held. Slide #73 is an example of this lesion.
Clinical Features1. Asymptornatic usually.
2. The usual appearance is a white, wrinkled or corrugated mucosa as seen in slide #73.
3. Gingival recession is also a common manifestation with cervical erosion of the teeth a less frequent finding.
Cause - Prolonged use of smokeless tobacco products such as snuff and chewing tobacco.
Histopathology - There is hyperkeratosis and mild hyperplasia (thickening) of the epithelium. Slide #74 is a low-power view showing hyperkeratosis and elongated rete ridges
Treatment - Progressive lesions or those that do not regress when there is cessation of the tobacco habit should be biopsied to rule out dysplasia or cancer. Hyperkeratotic lesions due to smokeless tobacco typically regress on cessation of the habit.Comment - Verrucous carcinoma and squamous carcinomas may arise in smokeless tobacco lesions. Organic carcinogens in the tobacco have been implicated. Usually at least 20 years of tobacco use is necessary to induce dysplastic or malignant change but several cases of cancer have been reported after less than 10 years of use.
14. ORAL MELANOTIC MACULES
(ephelis)
Two types: (A) Labial melanotic macule
(B) Oral melanotic macule
Clinical Features
1. These are brown-black lesions with a flat surface. Approximately 90% are solitary; multiple lesions are present in less than 10% of cases.2. Occurs equally in both sexes, mean age is 31.5 years with a range of 16 to 69 years. More than half are found in patients between the ages of 20 - 29.
3. May change in size and color over time.
4. Duration ranges from 2 months to 26 years with approximately 85% occurring on the lower lip and 15% on the upper lip, most are near the midline.
5. 85% of lesions are less than 0.5 cm, 15% are between 0.6 and 1.0 cm.
Cause - Unknown. It has been theorized that trauma may be a factor in some cases. Prolonged exposure to sunlight has also been implicated, but they do not change color with increased sun exposure as freckles do.
Histopathology - There is an increase in the amount of melanin in the basal cell layer of epithelium as shown in slide #76. The histology is similar to a freckle (ephelis) of the skin.
Treatment - No treatment is necessary. This lesion is benign and
has no malignant potential. Nevertheless, any pigmented lesion
that enlarges in size or deepens in color or becomes nodular or
ulcerated should be biopsied to rule out melanoma.
B. The oral melanotic macule is a pigmented lesion that occurs
Clinical Features
1. The lesions are either brown or varying combinations of blue, black, and brown.2. These lesions tend to occur in the fifth decade of life and the most common site is the gingiva.
3. The lesions are usually single and smaller than 1 cm. They may occur as multiple lesions.4. There is no sex preference.
Cause - Unknown. Oral pigmentation may be the result of racial pigmentation, endocrine disturbance (as in Addison's disease), antimalarial therapy and Peutz-Jeghers syndrome. Oral melanotic macules appear as freckles whereas the other forms of oral pigmentation usually are larger and more diffuse.Histopathogy- Same as for labial melanotic macule.
Treatment - None required. These lesions are not considered to be premalignant. However, lesions present fewer than 5 years and exhibiting changes in size or color, bleeding, ulceration or tumefaction, should be biopsied. It may be difficult to clinically differentiate a simple melanotic macule from an early melanoma.
15. AMALGAM TATTOO
During dental operative procedures or extractions, dental amalgam may accidentally become embedded in oral mucosa. It persists indefinitely as an area of blue to black pigmentation called an amalgam tattoo". Slide #78 shows a large area of pigmentation, The two primary molars had previously been restored with amalgam restorations and when they were prepared for chrome steel crowns, amalgam was inadvertently introduced into the mucosa adjacent to the teeth. Slide #79 shows an amalgam tattoo high on the alveolar mucosa of a patient who had an apicoectomy with an amalgam retrofill.
Clinical Features
1. They are asymptomatic, non-elevated, and usually of long duration.
2. They occur at any site, but gingiva is the most common location.3. Size is ordinarily less than 1 cm.
4. If the embedded particles are large enough, they may show up as radiodense (white flecks) on dental radiographs.
Cause - The accidental and usually unavoidable implantation of dental amalgam in oral soft tissues.
Histopathogy - Slide #80 is a medium-power view of oral mucosa showing specks of amalgam in the connective tissue. They appear as black particles. They may become aligned along small collagen fibers in the connective tissue, and basement membranes of small arteries and squamous epithelium. There is usually very little tissue reaction to the metal, occasionally there is mild fibrosis and inflammation.Treatment - No treatment is required. Amalgam tattoos Can usually be easily differentiated from melanotic macules, because of the slate gray coloration. When there is doubt between amalgam tattoo and a melanotic lesion, a biopsy would be indicated.
16. GEOGRAPHIC TONGUE
(benign migratory glossitis, glossitis areata migrans, wandering rash of the tongue)
Geographic tongue is a lesion of unknown cause characterized be
map-like, red areas on the dorsal, or lateral surface of the tongue. Slides
#81 and #82 are examples.
Clinical Features
1. Occurs in both sexes and all ages. Approximately 2% of the U.S. population is affected.2. Ordinarily asymptomatic, but occasionally a patient complains of burning sensation.
3. Lesions are usually multiple, found almost exclusively on the dorsal and lateral tongue mucosa. Rarely, this disease occurs on other mucosal surfaces. Lesions on ventral tongue are seen in Slide #83. Lesions on surfaces other than dorsal or lateral tongue have been called geographic stomatities or stomatitis areata migrans.
4. Lesions vary in size and are quite irregular in shape. Adjacent lesions may join to produce map-like areas.
5. Lesions are slightly depressed, redder than surrounding mucosa, and sometimes are outlined by a yellowish-white rim.
6. One of the outstanding features of this disease is the migratory nature of the lesions. Old lesions heal and new ones form giving the impression of migration.
Cause - Unknown.
Histopathology - The lesions are characterized by atrophy of finform papillae. A mild inflammatory reaction may be found in the lamina propria with migration of neutrophils into the epithelium forming small intraepithelial microabscesses. Slide #84 is a low power view. The yellowish-white perimeter seen clinically, when examined microscopically, proves to be a zone of parakeratosis with microabscesses. Microscopically, geographic tongue resembles psoriasis, however no convincing evidence confirms this association.Treatment - If lesions are asymstomatic no treatment is necessary. Burning sensation with geographic tongue may be associated with secondary candidiasis and antifungals may be beneficial. If fungus can be ruled out, topical steroids or antihistamines (diphenhydramine HCI suspension) are reported to relieve symptoms.
12. LICHEN PLANUS
Slides #85 and #86 show typical lesions on the buccal mucosa. Lesions of this disease appear in four forms: reticular, erosive, atrophic and plaque. The reticular type shows a pattern of lacy, white lines as shown in slides #85 and #86. In the erosive type, the same reticular pattern is seen, but there are areas of ulceration. An example of the erosive or ulcerative variety is seen in slide #87. The lacy pattern is lost in the plaque type; the lesions appear as a solid white macular or papular lesions (not shown). The atrophic form is most commonly seen on the attached gingiva and is often a diffuse erythematous lesion with erosion that causes discomfort.
Clinical Features
1. The lesion is found mostly in adults past age 40. Women are more often affected, approximately 2 to 1.
2. Lesions may occur on any area of the mouth; buccal mucosa is the most common site and typically, lesions are bilateral.3. The ulcerative type is painful: the reticular and plaque types, are ordinarily asymptomatic.
4. The disease is chronic, lasting months to years.
5. Typical lesions appear as a network of very slightly elevated white lines. These fines. have erroneously been called "striae of Wickham". If no striae are seen, you should be reluctant to make the diagnosis of lichen planus. (Other lesions such as hyperkeratosis or even squamous cell carcinoma may appear as a solid white plaque.)
6. Skin is more frequently affected than mucosa. Skin lesions appear as red, maculopapular, pruritic areas a few millimeters in diameter, The most common areas are the forearm and shins.
7. It has been reported that
approximately 1.5% of those with lichen planus will develop oral cancer. While this is some what contraversial patients should be followed closely and biopsied to confirm the diagnosis.
Cause - Lichen planus is thought to be a cell mediated immune disease. Antigens purportedly cause a proliferation of T-lympocytes which cause epithelial cytotoxicity. The antigens that provoke this reaction are unknown but some cases of lichen planus are thought to be caused by systemic medications-so-called lichenoid drug reactions. Antihypertensives, diuretics and non-steroidal or anti-inflammatories are commonly implicated but numerous other drugs may be causal.
Histopathology - The epithelial thickness ranges from thicker (hyperplastic) than normal to thinner (atrophic) , to ulcerative. Rete ridges are often thinner and more tapered than normal (sawtoothed rete ridges). The basal epithelial cells undergo necrosis leaving small holes (vacuolar change) and small eosinophilic bodies (colloid or Civatte bodies) in the basal cell zone. Slides #88 and #89 illustrate these changes. A band-like lymphocytic infiltration parallels the basement membrane and is important to the diagnosis.
Treatment - This disease requires no treatment unless it becomes ulcerated. In cases with ulceration, topical steroids such as triamcinolone or fluocinonide may be applied. However, if ulceration is too widespread, systemic prednisone is indicated. Topical Tretinoin 0. 1% has also been reported to be of benefit.
18. LEUKOPLAKIA/ERYTHROPLAKIA
Leukoplakia (white plaque) is a white, adherent lesion of mucosa. Because of the white color, it may be confused with other white
mucosal lesions Such as lichen planus and candidiasis. Leukoplakia lacks tile striae seen in lichen planus and unlike the white lesions of
candidiasis, it cannot be wiped off. Although this discussion is limited to oral lesions, leukoplakia may involve other mucosal surfaces such
as respiratory and genital. According to the World Health Organization leukoplakia. is defined as a white lesion that cannot be wiped off
and cannot be clinically diagnosed as another recognized entity.
Lesions of leukoplakia range in size from a few millimeters to those that cover exceeding large areas of the mouth. Slide #90 is a typical
example with lesions in the labial vestibule and floor of the mouth in a 51 year-old female. Leukoplakia is a disease of adults, rarely
affecting children. Men have the condition more often than do women.
The cause is not known, but tobacco and alcohol appear to be high risk factors. Physical trauma and vitamin A deficiency have also been
implicated.
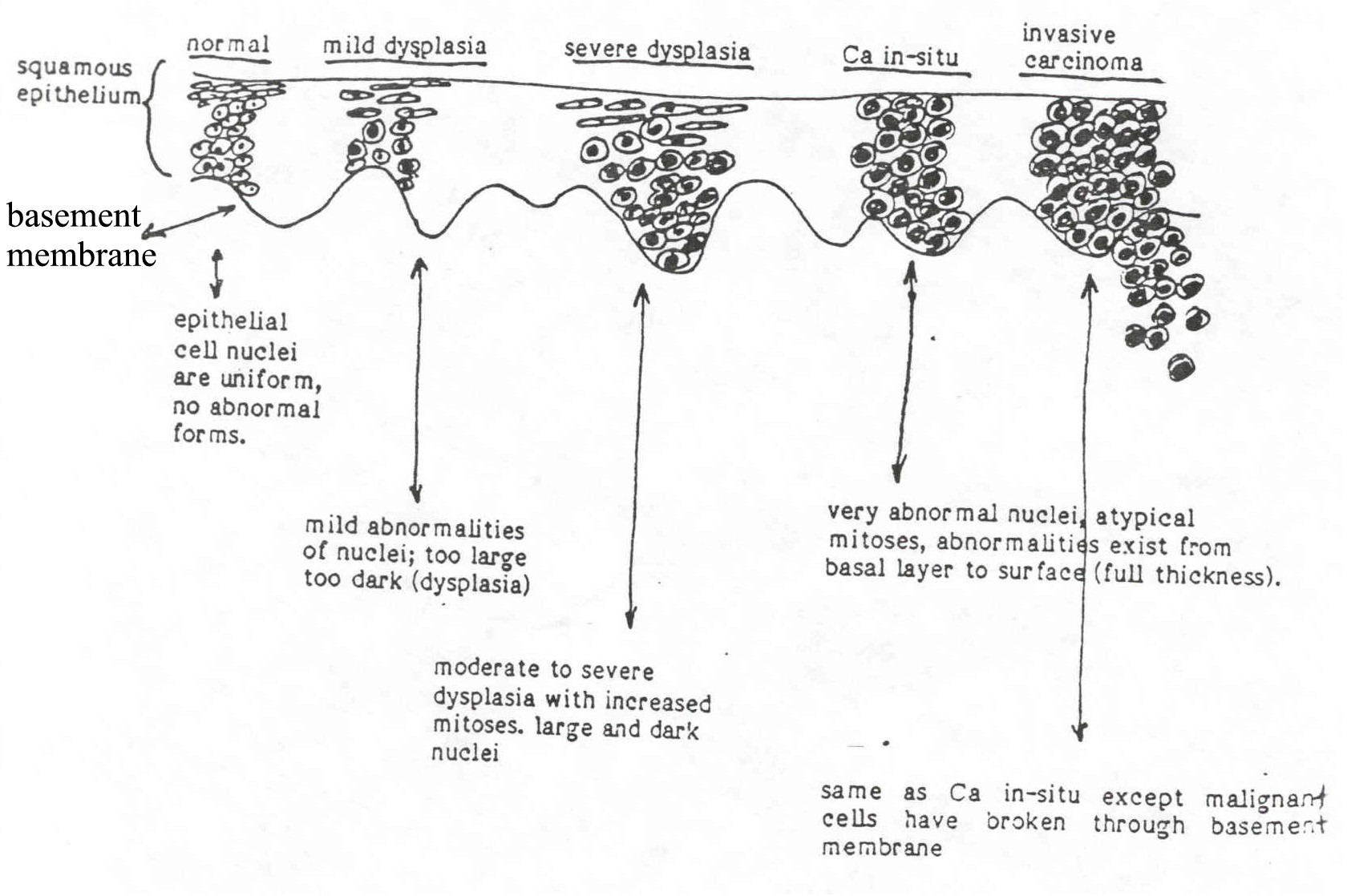
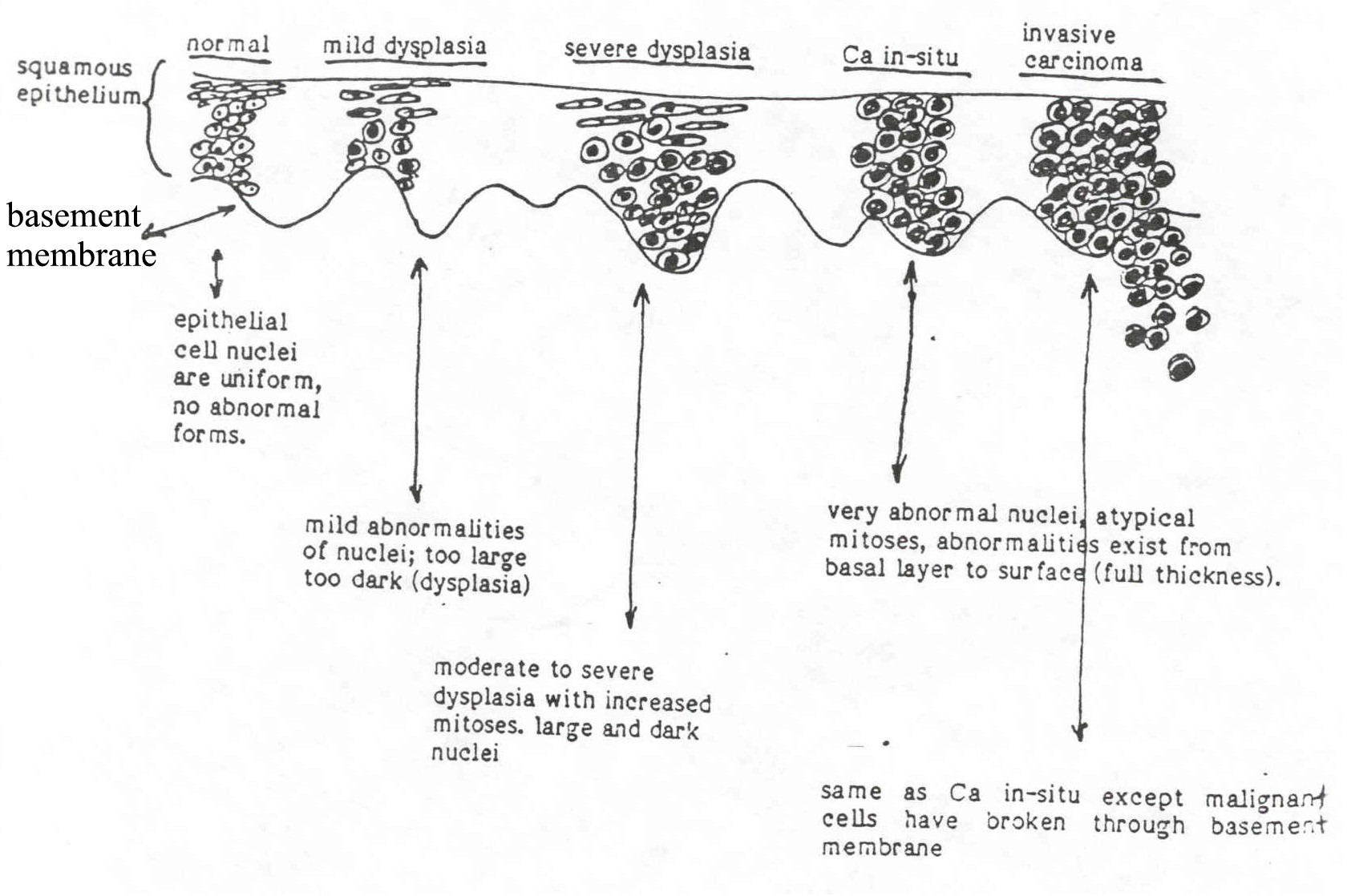
When examined microscopically, most cases of leukoplakia. are nothing more than hyperkeratosis as seen in figure #91. However, it
is important to remember that cancer (squamous cell carcinoma) may begin as leukoplakia. One study of over 3,000 patients with
leukoplakia showed that approximately 81 % were simple hyperkeratosis. However, twelve percent showed early precancerous changes
(dysplasia), 4% were carcinoma in-situ, and 3% were invasive carcinoma.
81 % - hyperkeratosis
12% - precancer (dysplasia)
4% - ca in-situ
3% - Invasive carcinoma
To illustrate, slide #92 is a 36-year-old female with leukoplakia involving most of the right ventral tongue. Microscopic study of this case
revealed severe cellular abnormalities (dysplasia), a precancerous lesion. Slide #93 is leukoplakia. of the lip in a 66-year-old female and
slide #94 is a photomicrograph of the same case. Nuclei of the squamous cells are larger
and darker than normal and there are increased mitoses, some of which
are abnormal. The cellular abnormalities involve the full thickness of is
the epithelium, but the basement membrane is still intact. This
combination of severe dysplasia with full-thickness involvement and intact
BM is referred to as carcinoma in-situ (in-situ = in-place). Slide #95 is
leukoplakia of the ventral tongue in a 50-year-old male. Biopsy showed
the same changes as seen in the previous case except the basement
membrane was no longer intact, and cancer cells have invaded into the
lamina propria.
The treatment of leukoplakia depends on the histologic finding as listed below:
Hyperkeratosis:
Removal not required, but patients should be followed and rebiopsied if it spreads. It is believed that approximately 4% of these patients will slip into the other categories within 10-20 years.
Dysplasia/Ca in-situ:
Involved area should be removed. Surgical excision is preferred, but lazer, electrocautery, and cryosurgery have been successfully employed.
Invasive cancer:
Superficially invasive cancers are ordinarily treated by surgery or radiation. Deeply invasive cancers are treated by extensive surgery including removal of regional lymph nodes. Radiation and chemotherapy are employed when there is doubt that surgery removed all the tumor.
*NOTE: Clinical leukoplakia (and erythroplakia) of the lateral and ventral tongue, floor of the mouth, and soft palate are more apt to be premalignant or malignant that are those located -in other sites such as hard palate, buccal mucosa and alveolar ridge.
ERYTHROPLAKIA (erythroplasia)
A persistent and unexplained red flat lesion is referred to as "erythroplakia". An example is shown in slide #96 involving the left soft palate, retromolar and posterior buccal mucosa. Many of the comments made about leukoplakia apply to erythroplakia. Age, sex, and risk factors are the same, Experience has shown that erythroplakia is much more likely to be cancerous or precancerous. One study found that 90% of clinical erythroplakias were cancers or precancerous. Therefore, biopsy is a virtual necessity. The red color is caused by thinning of the epithelium, especially the part of the epithelium overlying the dermal papillae. Combinations of leukoplakia and erythroplakia occur and have been referred to as "salt and pepper" lesions or more properly, "speckled leukoplakia". An example is shown in slide #97.
19. SQUAMOUS CELL CARCINOMA
(epidermoid carcinoma)
A wide variety of malignancies occur in the mouth such as adenocarcinomas of salivary gland origin, soft tissue sarcomas such as fibrosarcoma, and bone tumors such as osteosarcoma. The most common malignancy is squamous cell carcinoma derived from surface mucosa, accounting for more than 90% of all oral cancers. The cause of squamous carcinoma is unknown. Alcohol consumption and smoking increase the risk and sun exposure is a well-known factor in lip cancer. The human papilloma virus has been found in a significant number of carcinomas but its role in the cause of oral cancer is unclear.
Men are affected 3 or 4 times as often as women. Oral cancer is uncommon before the age of 40, but young adults and even children have been reported to develop oral squamous carcinoma. A suspicious lesion cannot be ignored simply because of the patient's youth.
Certain sites are more commonly involved. The same "danger zones" for leukoplakia/erythroplakia (soft palate, lingual gutter, lateral-ventral tongue and floor of mouth) are also high risk areas for cancer. About 75-80% of all mouth cancers arise in this horseshoe- shaped zone. The clinical appearance varies with the stage of the disease. The single most common appearance of early cancer is mixed leukoplakia/erythroplakia. Pure erythroplakia is the second most common appearance and leukoplakia is third. These have been illustrated under the previous sections on leukoplakia and erythroplakia. As the tumor grows, non-healing ulcers develop (fig #98 and #99) and eventually, a fleshy mass may form as seen in slides #100 and #101.
Although there is variation in histopathologic features, squamous carcinomas all have in common highly abnormal (dysplastic) cells with variation in nuclear size, shape, and increased staining intensity of the nuclei (hyperchromasia). Destruction of the basement membrane with invasion of the underlying lamina propria invariably occurs. Late in the disease, the lymphatic channels are invaded. This leads to spread (metastasis) to the regional (cervical) lymph nodes. Once metastasis has occurred prognosis is significantly reduced. The best chance for cure is early detection when lesions are less than 1 cm in size. When metastasis has occurred, efforts to achieve a cure include extensive surgery, radiation therapy, and sometimes chemotherapy.
Slide # 102 is a low-power picture of invasive carcinoma. Islands and cords of squamous carcinoma cells invade deep tissues on the left side of the Picture. Slide #103 is a high-power showing the highly atypical cellular and nuclear forms and abnormal mitoses. Most oral carcinomas are highly differentiated, i.e., the tumor cells still bear some resemblance to normal squamous cells. A small percent are poorly differentiated; the tumor cells bear little resemblance to normal squamous cells. In general, the poorly differentiated tumors have a worse prognosis than well diferentiated tumors.
The Outlook for survival depends on the stage of the disease at the time of diagnosis and treatment. in-situ lesions are 100% curable: Small (less than 2.0 cm diameter) tumors that are superficially invasive have about an 80% cure rate. As the tumor size and the depth of invasion increases, the prognosis worsens down to a miserable 25% 5-year survival for patients with larger, metastatic lesions. Although metastases to distant sites such as lung, brain, and bone marrow do occur, those who die of mouth cancer usually do so from the complications of local recurrence and cervical lymph node metastases rather than distant metastases.
20. PERIODONTAL DISEASES
A. GINGIVITIS
1. GINGIVITIS
Inflammation of the gingiva is among the mildest, but most common human ailments. Slide # 104 shows a patient with mild gingivitis; slide # 105 is of a more advanced case with large deposits of calculus.
Clinical Features1. With the possible exception of infants, gingivitis affects all ages and both sexes. It may be localized to involve the gingival of a few teeth or the entire gingiva may be affected.
2. The gingiva becomes smooth, glossy, and red; these are the cardinal signs of inflammation. The more severe the inflammation, the more swollen and red the gingiva becomes. Interdental papillae are edematous and rounded.
3. Labial and buccal gingiva are almost always affected more than the palatal and lingual gingiva.
4. Gingivitis is usually painless and chronic. The first thing the patient may notice is that the gingiva bleeds when brushing.
Cause - In almost every instance, gingivitis is caused by neglect of oral hygiene with the accumulation of bacterial plaque in interproximal areas and at the gingival margins.
Histopathology - Diagnosis is easily made by clinical examination.
If a biopsy were taken, you would see edema, vascular dilation,
and inflammatory cell infiltration, mostly chronic inflammatory
cells (lymphocytes and plasma cells, with a few neutrophils).
The bacterial toxins elaborated by plaque are thought
to seep into the gingiva to produce inflammation. One theory
proposes that bacterial proteases activate complement via the
alternate pathway. Certain fragments (C3a & C5a) in the
complement cascade inhance inflammation.
Treatment - Thorough dental prophylaxis followed by good home
care. The condition is completely reversible with no residual
damage.
Comment - Since you can scrape literally millions of bacteria from
the gingival sulcus of perfectly healthy mouths, it obviously takes
more than bacteria to cause gingivitis. There exists in all
of nature a delicate ecological balance. In health, the gingiva coexists in peace with oral flora. If the balance is tipped either by
increasing the numbers or virulence of the bacteria or
decreasing the resistance of the host, gingivitis ensues. Gingivitis
is reported to be of increased frequency during puberty and
pregnancy, and we have coined the terms "puberty gingivitis" and
pregnancy gingivitis" respectively. The exact role of gonadal
hormones in the pathogenesis of these forms of gingivitis is
unknown. On occasion, gingivitis produces enough edema and
inflammation to cause the gingiva to enlarge several times the
normal size. We then Call it "hyperplastic gingivitis". In this
condition there is overgrowth of gingival fibroblasts so the
enlargement is due to both fibrous hyperplasia and inflammation.
Slide # 106 shows a case of hyperplastic gingivitis in a 19-year-old
girl.
Several drugs including dilantin, calcium channel blockers
and cyclosporin have been shown to cause gingival fibrous
hyperplasia that resembles plaque induced hyperplastic gingivitis.
An example of dilantin hyperplasia is shown in slide # 107.
2. ACUTE NECROTIZING ULCERATIVE GINGIVITIS(Vincent's infection, trench mouth, ANUG)
This is a specific type of infection of oral mucosa in which lesions are found chiefly on marginal and papillary gingiva. It is not a contagious disease.
Clinical Features1. Necrosis of the interdental papillae that spreads to involve the adjacent facial and lingual marginal gingiva is virtually diagnostic of this disease. Slide # 108 is an example.
2. The ulcerated gingiva is covered by a creamy exudate or "pseudomembrane" that can be wiped off leaving a denuded, bleeding surface.
3. Patients have pain and halitosis and in severe cases, fever and cervical lymphandenitis.
4. Spread of lesions into the throat has been referred to as Vincent's angina. Destruction of large areas of mucosa in malnourished patients has been referred to as "noma".
5. ANUG occurs in all age groups, but is uncommon in children. It is a common occurance in those with HIV infection and is more common in smokers and those with emotional stress.
Cause - Treponema vincenth and Fusobacterium nucleaturn have been isolated from the lesions and are suspected as being the cause. Selenomonas and Prevotella intermedia organisms have also been implicated. Innoculations of these organisms into tissues of volunteers has not reproduced the disease, however. Reduction of host resistance is thought to play a role. Gaps obviously exist in our knowledge regarding the cause of ANUG.
Treatment - Treatment consists of debridement and cleaning the
teeth. In those patients with fever and cervical lymphadenids, an
antibiotic such as penicilin or metronidazole should be
considered. Topical anesthetics may provide palliation.
1. ADULT ONSET PERIODONTITIS
If gingivitis is untreated, the inflammatory, reaction will spread into deeper tissue, namely alveolar bone and the periodontal ligament. When this happens, we say the patient has periodontitis, The old term pyorrhea comes from the observation that in severe cases, suppuration occurs and "pus flows" (pyo=pus, rrhea=flow). Today we call it suppurative periodontitis if pus is present.
Clinical Features1. Affects both sexes and usually has onset in late teens or early twenties, but may not become clinically evident until the 30's and 40's. By age 45, about 35% of Americans are affected to some degree.
2. The earliest detectable lesion is loss of interdental alveolar bone. Bone loss starts at the alveolar crest so that bone height around the teeth is decreased. Because you cannot see bone by clinical examination, X-ray is the best way to detect early periodontitis. As bone recedes, the depth of the gingival sulcus increases. This can be detected clinically with a periodontal probe. With more advanced disease sufficient bone loss occurs to cause tooth mobility and migration. Slide # 109 is a film showing slight bone loss (early periodontitis) . Slide # 110 shows moderate bone loss, and slide # 111 shows extensive bone loss (advanced periodontitis)
3. Since periodontitis is a sequelae of gingivitis, most patients with periodontitis will also have gingivitis.
4. Periodontitis is a fairly symmetric disease affecting all areas
of the alveolar bone equally, but it may be worse in some areas than in others. This even destruction of
bone around all teeth has been referred to as the "horizontal" pattern of bone loss.
5. With progressive bone loss, the epithelial attachment of
the gingiva to the tooth migrates apically down the root of the
6. The bone loss is with few exceptions irreversible. Procedures such as grafting of bone or synthetic materials may be helpful in restoring some of the lost bone.
7. Periodontitis is the single largest cause of tooth loss, dental caries ranks second.
Comment - Bacterial plaque is thought to be the cause of
periodontitis.
Histopathology - Human material is scarce. To get a
histopathologic "look" at periodontitis would require taking a tooth
(or teeth) along with a surrounding block of bone. Much of what is
known about periodontitis comes from animal studies and human
material taken at autopsy. Suffice it to say, there is chronic
inflammation in the involved bone, periodontal ligament, and
gingiva, coupled with osteoclastic bone resorption and gradual
displacement of the epithelial attachment down the root of the
tooth.
Treatment - Depends on the severity of the disease. The disease
cannot be cured (restored to normal) but can be arrested, In mild
cases with little bone loss, thorough cleaning of teeth (scaling and
root planing) coupled with good oral hygiene is enough to arrest
the disease. In more severe cases with extensive bone loss, scaling
and root planing plus surgery to eliminate "pockets" is necessary.
Pockets are a nidus for infection that the patient can't keep clean.
In severe cases there may be no choice but to extract the teeth.
The best treatment is prevention.
Comment - A subtype of adult onset periodontitis has recently been described* and has been referred to as "rapidly advancing periodontitis" or "RAP". This disease is characterized by accelerated bone loss occurring over a period of weeks to months rather than years. In this form of periodontitis, there is evidence of increased activity of Porphyromonas, Actinobacillus, Eikenella, and Prevotella organisms coupled with defects of leukocyte chemotaxis.
*Page, R., Rapidly Advancing Periodontitis. J. Periodontology. 54:197, 1983.
2. JUVENILE PERIODONTITIS (formerly periodontosis) Slides # 112 and # 113 are examples of this disease.
Clinical Features
1. This disease typically, affects teenagers.2. JP is characterized by destruction of alveolar bone around only first permanent molar teeth and incisor teeth.
Cause - Research has implicated an array of gram-negative,
anaerobic rods, especially Actinobacillus actinomycetemcomitans.
There is no plausible explanation for the selective involvement of
the first molar and incisor teeth other than the "first erupted-first
involved" theory.
Histopathology - Same as for adult onset periodontitis, namely non-specific periodontal inflammation.
Treatment - Scaling and root planning combined with antibiotic therapy is the best treatment.
Note: That form of JP affecting only first permanent molars and incisors
has been referred to as localized JP. A form affecting all permanent teeth
has been referred to as generalized JP. Both are uncommon, but LJP-is
the more common of the two.
3. PREPUBERTAL PERIODONTITIS (Slide # 114 is an example of this disease.)
Clinical Features1. Prepubertal periodointitis is a disease affecting deciduous teeth in children around the age of 4 to 8 years. It is rare.
2. Radiographs show mild to severe loss of alveolar bone around deciduous teeth.
3. Gingiva may be normal or inflamed.
Cause - An abnormality in the immune system in the form of decreased chemotaxis of monocytes and neutrophils has been described.
Treatment - Good oral hygiene is a must, but there is no known way to improve chemotactic and phagocytic capabilities of macrophages and neutrophils.
Comment - Histiocytosis X (Langerhans' Histiocytosis) and Burkitt's lymphoma should be considered in the differential diagnosis, the radiographic appearance may be identical to prepubertal periodontitis. Children with prepubertal periodontitis coupled with hyperkeratosis of the palms and soles are said to have the Papillon-Lefevre syndrome. Prepubertal periodontitis has also been described in children with Ehlers-Danlos syndrome.
21. DENTAL CARIES
Differential diagnosis is not a problem because caries is the only disease that attacks the outer surface of a tooth. Slides # 115 and # 116 show typical carious lesions.
Clinical Features1. Pit and fissures on the occlusal surface of posterior teeth are extremely susceptible (pit and fissure caries).
2. Smooth surface caries usually start on the gingiva one-third of the labial (and less often the lingual) surface of a tooth.
3. Just below the contact point on the proximal surface is another area that frequently becomes carious. The earliest sign is a small white spot (decalcification) that soon becomes a yellow-brown color. Cavitation follows.
Radiographic Features
1. Radiographs are useful in detecting caries on those surfaces that cannot be seen clinically. (Slide #117).2. Early interprosimal caries usually presents as a "small scooped out" radiolucent area in the enamel or sometimes as a triangular lesion with the apex pointing to the DE junction.
3. When caries reaches the dentino-enamel junction, it spreads
laterally and undermines overlying enamel.
2. Dental Hygiene - One of the most important factors. Clean
3. Diet - High carbohydrate diet favors high caries rate.
4. Tooth composition - High fluoride content improves
5. Saliva - Normal volume, bacteriostatic constituents,
Histopathology - In enamel, caries follows the enamel rods. You
Cause - Caries is an infectious disease caused by several bacteria. Streptococcus mutans is thought to be the most important
organism in crown caries. In the presence of dietary sucrose, S. mutans secretes an extracellular polysaccharide (glucan or
dextran) that adheres to teeth and forms a matrix favorable for bacterial colonization and adherence. The glucan is produced by
the action of the enzyme glucosyltransferase, and is water insoluble. Bacterial metabolism causes acid accumulation
that leads to demineralization of tooth structure. Demineralization exposes the protein matrix of the tooth to
digestion by proteolytic organisms and a cavity forms. Actinomyces species are regarded
A plethora of factors serve to promote or retard dental decay,
They are:
1. Heredity - Long suspected, but still not proved to be a factor
in caries. So many things, mostly environmental, affect
caries so that it is difficult to determine the influence of heredity.
Treatment - Prevention through good oral hygiene, proper diet, and
regular dental care. For those patients with xerostomia daily home
fluoride application is recommeded. When a carious lesions
extends into dentin the only treatment is restorative dentistry. If
untreated, dental caries usually leads to inflammation of the pulp (pulpitis).
22. PERIAPICAL GRANULOMA/PERIAPICAL CYST
The periapical granuloma (dental granuloma, chronic apical
periodontitis) is one of the most common lesions in dentistry. It is a focus
of chronic inflammation around the apex of a tooth and is a sequelae of pulpitis. Slide # 120 is a radiograph of a typical granuloma. Periapical
cysts are radiographically similar to granulomas and they have a common
pathogenesis. The major difference between granulomas and cysts is the
presence of an epithelial lined central cavity in the cyst. Slide # 121 shows
an example of a periapical cyst. Since the clinical features, radiographs,
and treatment are the same for both lesions, they will be discussed as one. It should be noted that a granuloma may become a cyst or abscess and an
abscess may develop into a granuloma.
1. Patients are usually asymptomatic, but occasionally there is pain. The affected tooth. may be tender to percussion.
2. An asymptomatic lesion present for years may undergo an acute reinfection leading to suppuration (abscess formation) With extreme pain. An abscess may lead to acute osteomyelitis or cellulitis.
3. If suppuration does occur, the pus may extend through bone and periosteum to the gingiva. This small gingival accumulation of pus produces a fluctuant swelling referred to as a parulis or gum boil.Radiographic Features
1. Always occur at or near the apex of a tooth with pulpitis. They are purely radiolucent.
2. Size ranges from a few millimeters to 2.0 cm.
3. Small lesions -usually show no appreciable resorption of root tips. However, larger granulomas and Cysts may exhibit root resorption that may simulate a tumor. Remember that in granulomas and cysts the tooth always has pulpitis and is non vital. The crown almost always shows caries, a restoration or a root canal filling.
Cause - Both the granuloma and the cyst are direct sequelae of inflammation of the pulp that has extended into the periapical tissues. On rare occasions, trauma rather than dental caries may be a cause of granulomas and cysts.
Histopathology
Granuloma - This lesion consists of fibroblasts, capillaries, and inflammatory cells. Neutrophils, lymphocytes and plasma cells are found in varying proportions. Lipid laden histiocytes (foam cells) are usually present. Cholesterol crystals accumulate, but are chemically dissolved during slide preparation (cholesterol clefts). Hemosiderin pigment may be seen.Cyst- The cyst is a sac, sometimes containing fluid. The wall is composed of inflamed fibrous connective tissue and the inner surface is lined by stratified squamous epithelium (slide # 122). The epithelium is derived from
rests of Malassez, and the inflammation is usually chronic and composed of lymphocytes, plasma cells and macrophages.Treatment - Treatment consists of endodontic therapy or extraction of the offending tooth.
Comment - Periapical abscesses, granulomas and cysts arise when a pulp inflammation extends into the periapical tissues. Whether or not there is bacterial invasion of the periapical tissues is controversial. Some literature suggest that bacteria are confined to the pulp whereas others believe the bacteria actually invade the periapical tissue. A lengthy discussion is beyond the scope of this study set, but students should know of the controversy and be aware that a sizable body of literature can be found on the subject.
23. CONDENSING OSTETTIS
(focal sclerosing osteomyelitis)
Condensing osteitis is a reaction to dental infection. It differs from periapical granuloma and cyst in that there is bone production rather than bone destruction. Slide #123 is an example of condensing osteitis.
Clinical Features
1. More commonly seen in the young and seems to show
special predilection for the periapical region of lower molars,
especially first molars.
2. The associated tooth is usually carious or contains a large
3. May be asymptomatic or there may be symptoms of pulpitis (pain).
4. Current levels of knowledge suggests that the pulp is irreversibly in flamed.Radiographic Features
1. A radiodensity of about 1.0 cm or less surrounds the apex of the infected tooth. The density may be sharply defined or gradually fade into the surrounding normal bone.
Cause - The cause is pulp inflammation caused by trauma. The inflammation spreads to apical, periodontal tissues stimulating new bone production.
Histopathology - No slides will be shown since there is no reason to biopsy this lesion to arrive at a diagnosis. Those who have biopsied this lesion report it consists of dense bone with variable amounts of chronic inflammation in the marrow spaces.
Treatment - The treatment is endodontic filling or extraction.
Comment - It is believed (with little evidence) that condensing is osteitis results when the causative organisms are of low virulence and host resistance is high. The reverse is believed to lead to granuloma and cyst formation. This condition must be differatiated from osteosclerosis (idiopathic sclerosis) which may appear radiographically similar but is associated with vital teeth.
24. DENTIGEROUS CYST
(follicular cyst)
This is a developmental cyst that forms around the crown of an unerupted tooth. This cyst is thought to occur when fluid accumulates in the space between the tooth surface and the epithelium of the reduced enamel organ. Slide # 124, # 125, # 126 and # 127 are examples of dentigerous cysts.
Clinical Features1. Occurs in all ages, but most often in young adults.
2.They are usually asymptomatic and discovered on routine dental films. In the mandible, compression of the inferior alveolar nerve may cause paresthesia.
3. In some cases, a dentigerous cyst will cause expansion of the jaw.
Radiographic Features
1. This cyst is always associated with the crown of an unerupted tooth. Slide #126 shows the relationship of the cyst and the associated tooth.
2. The mandibular third molars and, the maxillary canines are the teeth most often affected. Deciduous teeth are
infrequently affected.
3. Dentigerous cysts are purely radiolucent and are usually
5. This cyst will displace the associated tooth, sometimes great distances from the normal location in the mandible, the associated tooth may be pushed to the condyle or it may be found at the inferior border of & ie body of the mandible. In the maxilla, the tooth may be displaced to a location near the orbit.
25. NASOPALATINE DUCT CYST
(incisive canal cyst)
This is a cyst of developmental origin arising in the incisive canal,
Slide # 129 is an example of such a cyst.
Clinical Features
1. These cysts are almost always asymptomatic and are usually discovered on routine dental films where they appear as oval, or heart-shaped radiolucent lesions in the vicinity of the maxillary central incisors.
2. They are usually found in adults.
3. Adjacent teeth are vital and seldom is there displacement or resorption of the teeth roots.
Cause - This is a developmental cyst presumably arising from epithelial remnants of the nasopalatine duct.
Histopathology - The cyst consists of a wall of fibrous connective tissue rich in blood vessels and peripheral nerves. The lumen is lined by squamous epithelium , respiratory epithelium or combinations of these.
Treatment - Surgical enucleation.
Comments - There is a tendency to over-diagnose this cyst. A
funnel shaped opening of an otherwise normal incisive canal may
radiographically cast a shadow that resembles a small NPD cyst.
(periapical cemental dysplasia)
26. CEMENTOMA
Clinical Features
1. Cannot be detected by clinical examination. They are discovered on radiographs.
2. This condition is more common in black women.3. Adults are more often affected: exceedingly rare in children.
4. The apices of the mandibular anterior teeth are the most common site.
5. May occur as a solitary lesion, but multiple lesions are not uncommon.
6. Always asymptomatic.
Radiographic Features1. The X-ray appearance varies according to the age of the lesion. "Young" or first stage lesions are purely radiolucent. This is said to be the "osteolytic" stage since there is periapical proliferation of fibrous connective tissue with resulting bone resorption. Slide # 130 shows a patient with several cementomas in the early or "osteolytic" stage.
2. Eventually, the growth stops and the lesion forms cementum in the central portion. X-ray examination of this 2nd stage shows a central radiodensity with a radiolucent halo. Most of the cementomas we see- are in this stage. (slide#131)
3. With time, cementum becomes deposited throughout the
entire lesion. The lesion is now "burned-out" (stage 3)and is
said to be "mature".
Cause - Unknown.
Treatment - There is no treatment required.
Comment - Stage one cementomas may radiographically resemble
a small periapical granuloma or cyst. The major difference is that
cementomas are found at the apices of vital teeth. Some patients
develop multiple comentoma-like lesions throughout the jaws.
This is referred to as florid osseous dysplasia.